To determine the nutritional adequacy of a tube feeding – Determining the nutritional adequacy of tube feeding is paramount for individuals relying on this method of nutrient delivery. This comprehensive guide explores the multifaceted aspects of tube feeding, encompassing nutritional assessment, energy and protein requirements, formula composition, monitoring and evaluation, and strategies for adjustments and modifications.
By delving into these essential elements, healthcare professionals can optimize nutritional outcomes for patients receiving tube feeding.
Nutritional assessment forms the cornerstone of ensuring adequate nutrient intake. It involves evaluating key parameters such as anthropometric measurements, biochemical markers, and dietary intake. Energy and protein requirements vary based on individual characteristics and underlying medical conditions, necessitating careful calculation and monitoring.
Nutritional Assessment
A thorough nutritional assessment is crucial for individuals receiving tube feeding to ensure their nutritional needs are met. This assessment evaluates various parameters, including:
- Anthropometric measurements (e.g., weight, height, body mass index)
- Biochemical parameters (e.g., serum albumin, prealbumin, electrolytes)
- Dietary intake (e.g., type and amount of tube feeding formula)
- Medical history and current health status
| Nutritional Parameter | Indicator |
|---|---|
| Energy | Caloric intake, resting energy expenditure |
| Protein | Nitrogen balance, serum albumin |
| Carbohydrates | Blood glucose levels, glycosylated hemoglobin |
| Fats | Serum lipid levels, essential fatty acid status |
| Vitamins and Minerals | Serum levels, intake from tube feeding formula |
Energy and Protein Requirements: To Determine The Nutritional Adequacy Of A Tube Feeding
Energy and protein requirements for individuals receiving tube feeding vary depending on factors such as age, activity level, and medical condition. The estimated energy requirement (EER) can be calculated using the Harris-Benedict equation, while protein requirements range from 1.2-2.0 grams per kilogram of body weight per day.
| Patient Population | Energy Requirements (kcal/kg/day) | Protein Requirements (g/kg/day) |
|---|---|---|
| Critically ill patients | 25-30 | 1.5-2.0 |
| Stable patients | 20-25 | 1.2-1.5 |
| Children | 80-100 | 1.5-2.0 |
| Elderly patients | 18-22 | 1.2-1.5 |
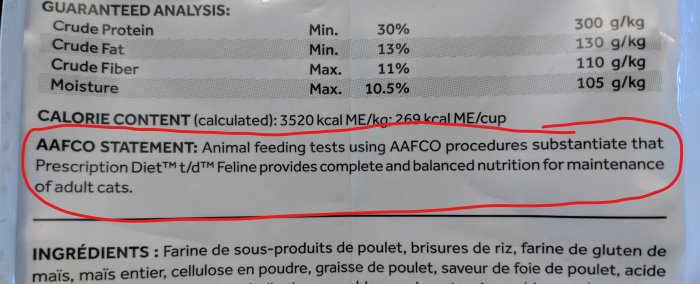
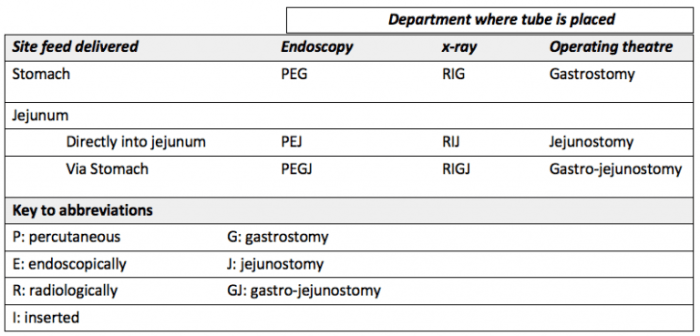
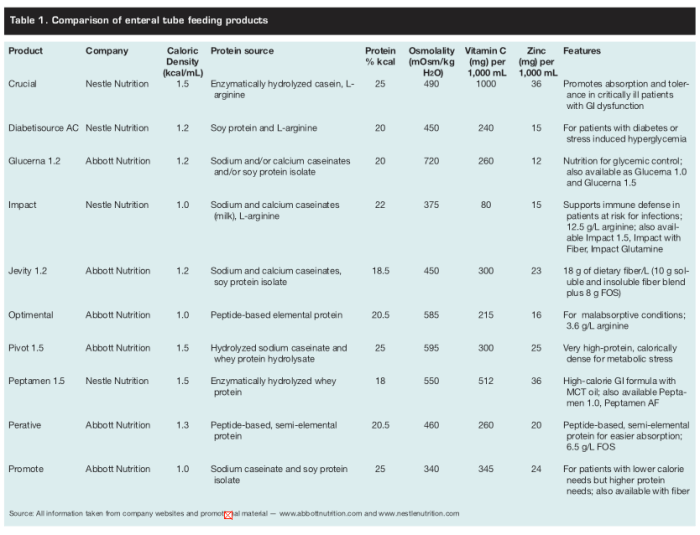
Nutrient Composition of Tube Feeding Formulas
Tube feeding formulas are designed to provide a complete and balanced nutritional intake. They vary in their composition, including:
- Macronutrients:Carbohydrates, proteins, and fats
- Micronutrients:Vitamins and minerals
- Electrolytes:Sodium, potassium, chloride, etc.
| Nutrient | Role |
|---|---|
| Carbohydrates | Primary energy source |
| Proteins | Tissue repair and maintenance |
| Fats | Energy storage, essential fatty acid provision |
| Vitamins | Coenzymes and cofactors for metabolic processes |
| Minerals | Bone health, electrolyte balance, enzyme function |
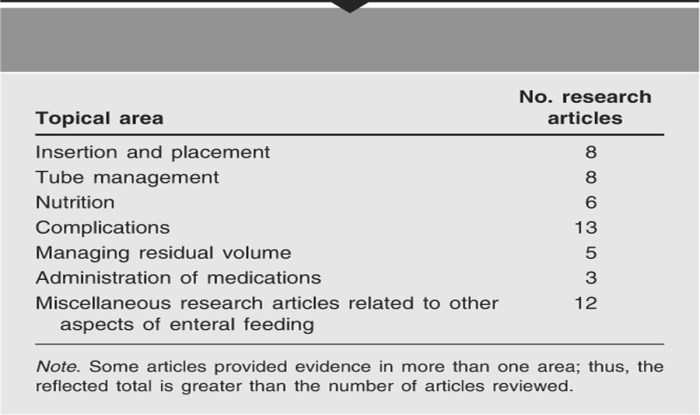
Monitoring and Evaluation
Regular monitoring is essential to ensure the nutritional adequacy of tube feeding. Parameters to be monitored include:
- Weight and other anthropometric measurements
- Biochemical parameters (e.g., serum albumin, prealbumin)
- Dietary intake
- Clinical signs and symptoms (e.g., edema, muscle wasting)
Potential Signs and Symptoms of Nutritional Inadequacy:
- Weight loss or gain
- Muscle wasting
- Edema
- Fatigue
- Skin problems
Adjustments and Modifications
Adjustments to tube feeding regimens may be necessary to ensure nutritional adequacy. Factors that may necessitate adjustments include:
- Changes in medical condition
- Changes in activity level
- Inadequate weight gain or loss
- Biochemical abnormalities
Process of Making Adjustments to Tube Feeding Regimens:
- Assess nutritional status and identify any deficiencies
- Adjust the type or amount of tube feeding formula
- Add supplements or medications as needed
- Monitor and evaluate response to adjustments
FAQ Resource
How often should nutritional assessment be conducted for individuals receiving tube feeding?
Nutritional assessment should be conducted regularly, typically every 1-2 weeks initially, and then adjusted based on individual patient needs and stability.
What are the key indicators of nutritional inadequacy in tube feeding?
Potential signs and symptoms of nutritional inadequacy include weight loss, muscle wasting, fatigue, electrolyte imbalances, and impaired wound healing.
How are energy and protein requirements determined for individuals receiving tube feeding?
Energy and protein requirements are calculated based on factors such as age, weight, activity level, underlying medical conditions, and stress levels.